Inguinal hernia repair techniques have evolved over centuries, as knowledge of groin anatomy has improved. Inguinal hernia descriptions and ways of treating them were mentioned by ancient civilizations, including Egyptians, Phoenicians, Greeks, and Romans. However, most advances took place in the Modern Era, with many open tissue repair techniques being developed and most eventually falling out of favor. Some of the most notable ones are Bassini, McVay, Halsted and Shouldice. Of note, some of the “no mesh” techniques employ the use of steel wire or Prolene permanent suture, resulting in significant retained foreign body that may even rival some available mesh products on the market. Tissue repairs aim to close the hernia defect (a hole in the muscle) with sutures, thus creating unphysiological tension in the groin, which is likely responsible for increased patient disability and higher recurrence rates.
To mitigate these factors, mesh use for open inguinal hernia repairs became popular in 1980’s. The gold standard technique for open inguinal hernia repair is the Lichtenstein repair, which was developed in 1984-1988. This is a “tension-free” repair, in which the hernia defect is covered with a flat prosthetic material that overlaps the defect for a few centimeters in all directions. Improvements of the Lichtenstein technique were later made by Dr. Parviz Amid from UCLA, to help decrease recurrence rates even more, and minimize the chance of chronic groin pain after surgery.
Nonetheless, open inguinal hernia repairs still led to significant pain and disability. Minimally invasive techniques for hernia repairs emerged in the 1990’s, when laparoscopy gained traction for other general surgery procedures. Two techniques were further refined: TEP (total extraperitoneal approach) and TAPP (transabdominal preperitoneal approach), which are still performed today. These techniques involve reinforcing the weakened inguinal floor with mesh from the inside in a “tension-free” fashion (a frequently used analogy is patching a tire from the inside with laparoscopy, as opposed to patching it on the outside with open repairs – the intraabdominal pressure makes the patch stick better to the defect in the laparoscopic repair and may push it away in the open repair). Lastly, robotic inguinal hernia repair was popularized in the 2000’s by extending the principles of the TAPP repair to the robotic technology. The robotic technique is widely applied in the U.S. and other places around the World today.
For more information about the history of inguinal hernia repair, we recommend reading the following article written by Dr. Edward Felix, one of the pioneers of the laparoscopic approach:
As mentioned, no-mesh (tissue repair) are rarely used nowadays as primary operations due to the high recurrence rates. However, many patients are concerned with the use of mesh and wonder what the most appropriate material for minimally invasive hernia repair is. We will break up this question in a few small topics.
“Is mesh safe for inguinal hernia repair?”
The answer is: Yes. Mesh repairs represent the standard of care for inguinal hernia repair. The Mesh Advisory Statement for Patients by the American Hernia Society reinforces this point.
“What meshes can be used for inguinal hernia repair?”
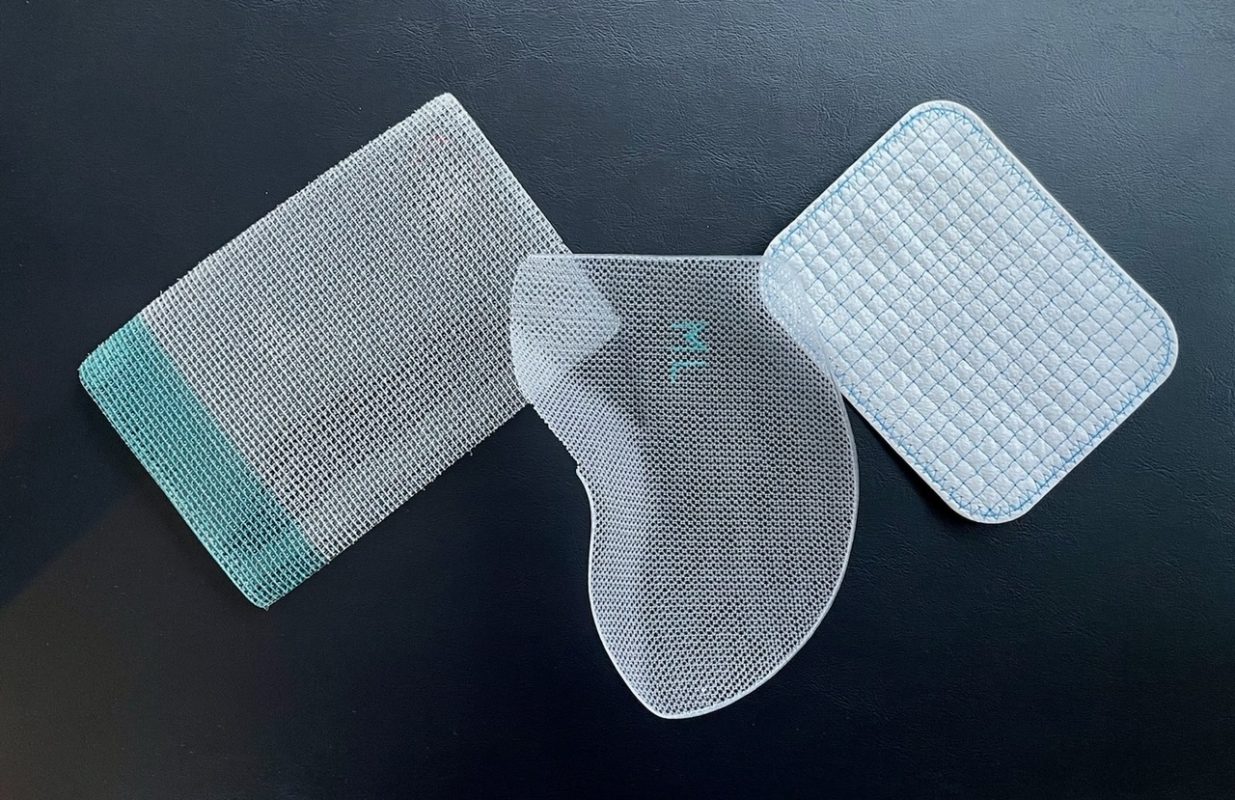
There is a wide array of meshes available on the market, and in a recent survey we performed with surgeons around the World, we identified over 25 different prosthetic materials implanted for laparoscopic and robotic inguinal hernia repairs. Most surgeons use a synthetic permanent material, generally polypropylene or polyester. There is no data to suggest that any of the two is superior to the other one. A light-weight or medium-weight material is generally appropriate for most patients, and these offer enough support with decreased fibrotic reaction and foreign-body sensation, when compared with the use of a heavy-weight material. Some of the most commonly used materials for laparoscopic and robotic hernia repairs include ProGripTM Laparoscopic Self-Fixating mesh, DextileTM Anatomical mesh, and Bard 3D MaxTM MID mesh . The former is a light-weight polyester mesh with resorbable grips on one side (like Velcro), which facilitates adherence of the mesh to the muscle and alleviates the need to use suturing or other fixation devices. The latter ones are polypropylene medium-weight meshes shaped to conform to the anatomy of the pelvis.
“Can resorbable mesh be used for minimally invasive hernia repair?”
Short answer: Yes. However, once the mesh is resorbed, the hernia would come back if the hole in the muscle (hernia defect) is left alone as in the standard technique. To mitigate this, the hole can be closed with sutures (creating some tension) and then the inguinal floor reinforced with a resorbable mesh. Caution should be used, as closure of the defect has the potential of entrapping nerves in the sutures, leading to chronic groin pain. This is not the standard of care but can be performed in patients who are completely against the use of synthetic (permanent) mesh.
“Are there any other mesh alternatives?”
Yes. Some companies produce hybrid meshes. One such example is TELA Bio. Their product, Ovitex , has a permanent scaffold made of polypropylene, and a resorbable collagen component, made of sheep rumen (stomach). This mesh reduces the synthetic material burden in the groin, but still offers some means of permanent reinforcement once the collagen is resorbed. The procedure has been popularized as the ReBAR (Reinforced Biologic Augmented Repair) Technique.
The company maintains an informative website about mesh repairs and alternatives to synthetic mesh: https://abouthernia.com
“Can an inguinal hernia be repaired robotically without mesh?”
Yes, in very few selected cases, but this does not represent the standard of care. The hernia defect can be closed with sutures creating a tension repair. It can be done in thin patients with small defects. A single case series of 13 patients has been published by Dr. Shirin Towfigh from Los Angeles.
Lastly, official information about mesh can be found on the FDA website:
https://www.fda.gov/medical-devices/implants-and-prosthetics/hernia-surgical-mesh-implants
We hope you found this information helpful. If you would like to discuss any of the points above in more detail, please schedule an appointment with Dr. Lucian Panait.